News & Highlights
Topics: Clinical & Translational Research, Funding, Pilot Funding
Senses and Sensibility: Experiencing the World Around Us
Ten investigators awarded pilot funding for projects focused on the senses.
Eating a delicious meal, listening to music, watching a movie, or performing everyday activities such as walking or engaging in conversation with co-workers – all these activities rely on the mechanisms of our senses. Our senses allow us to connect to the world around us, perceive our environment, and interact with other people. There are five senses commonly understood–sight, touch, taste, hearing, and smell–as well as two others, vestibular and proprioception.
To advance research in this area, we opened a funding opportunity in October 2021, soliciting proposals from Harvard University-affiliated researchers. Investigators were invited to submit projects related to any aspect of sensory perception or the human sensory system, including projects focused on the vestibular, proprioception, and other sensory systems. Each of the 10 awarded projects received $50,000 for one year.
Any disruption of our senses can limit our interactions with the world around us or make it harder to perform certain activities. For example, hearing loss can make it more difficult to follow conversations and a reduction in vision may make driving impossible, while a balance disorder can limit safe movement. Proprioception is the internal sense of body position; it monitors where our bodies are in space so that we can move our hands or feet without having to observe them. The vestibular system is responsible for maintaining our sense of balance and monitoring the sensation of orientation and acceleration of our heads in any direction.
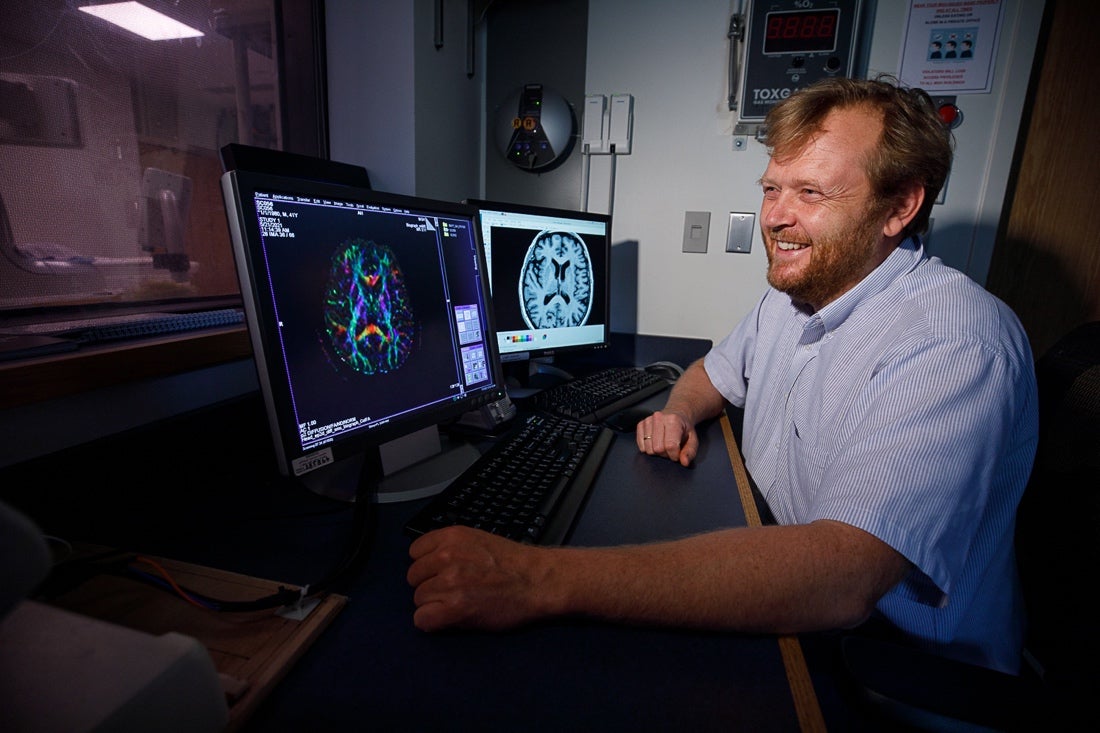
Nearly 50 applications were received, covering topic areas ranging from diagnosing dizziness using balance biomarkers to using an all-in-one diagnostic test to identify the bacteria which causes an eye infection that can lead to uveitis, to detection of hidden hearing loss using advanced diffusion magnetic resonance imaging (MRI).
“Through this pilot funding from Harvard Catalyst, we can now compare this new intervention to a placebo, the next necessary step towards establishing mirror therapy as a treatment option for people who suffer from tinnitus.”
Tinnitus is a health condition addressed in one project, which affects one in 10 adults. Responding to the need for safe, accessible, and affordable therapies, Clas Linnman, PhD, assistant professor at Spaulding Rehabilitation Hospital, will be using his pilot funding to investigate the use of an auditory mirror therapy as a treatment. Linnman’s study concept borrows from the treatment of phantom limb pain in amputees which uses mirror box therapy. In this therapy, a mirror gives the visual illusion of an intact limb to amputees, which allows the brain to reinterpret the lack of sensory nerve signals.
Building on this concept, a pair of headphones switch the communication of left and right sounds, so sounds from the left are heard as if they are on the right, and vice versa. The effect is that one must rely completely on vision rather than on sound to localize where the sound is coming from.
“Through this pilot funding from Harvard Catalyst, we can now compare this new intervention to a placebo, the next necessary step towards establishing mirror therapy as a treatment option for people who suffer from tinnitus,” said Linnman.
If successful, this therapy could become a treatment option that is non-invasive and safe, with the possibility of providing relief to the many adults who suffer from this condition.
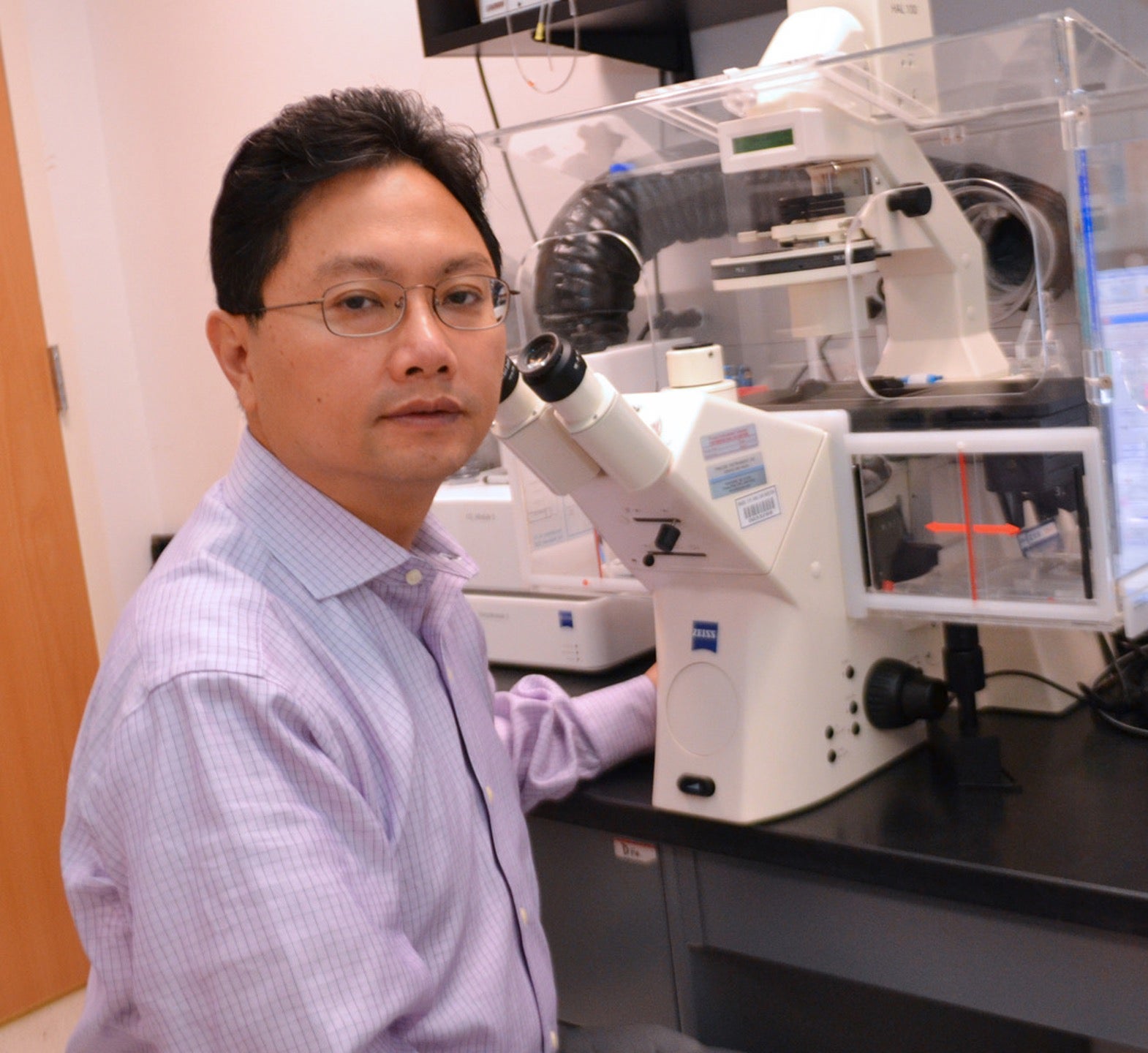
Another project focuses on cochlear hair cells, which are the sensory cells that detect sound. One of the most common causes of permanent hearing loss is the irreversible damage and loss of these inner ear cells. Innovative strategies are needed to regenerate these cells and recover hearing. Zheng-Yi Chen, MD, associate professor at Massachusetts Eye and Ear (MEE), recently discovered that the coactivation of two genes, Myc and Notch1, with a transcription factor called ATOH1, was enough to regenerate hair cells and reprogram the cochlea in adult transgenic mice.
“We believe we are at the cusp of using regeneration as future treatment for hearing loss without any drug therapy,” said Chen. “This funding allows us to optimize our drug-like approach for inner ear hair cell regeneration, providing us a critical step towards moving this discovery to clinical application.”
Chen and his team will next apply a cocktail of drug-like molecules (e.g., siRNA) to induce hair cell regeneration in the mouse’s damaged inner ear and examine the extent to which hearing can be restored using these cells.
Another awarded project focuses on the sudden loss of taste and smell, one of the most puzzling and unique symptoms of COVID-19, which 68% of people who have had COVID-19 experienced, as reported by observational studies. This loss of taste and smell is transient for most people who have contracted the virus. Approximately 45% of patients go on to partially recover their sense of taste and smell. However, approximately 4% of patients who had COVID-19 experience loss or disruption of taste and smell for up to six months after recovery.
“This funding allows us to optimize our drug-like approach for inner ear hair cell regeneration, providing us a critical step towards moving this discovery to clinical application.”
These data led Lora Bankova, MD, assistant professor at Brigham and Women’s Hospital, to the possibility that severe damage to nasal epithelial cells could be responsible for the long-lasting loss of smell in COVID-19 patients.
“When we launched our study, our plan was to conduct a small sample of fewer than 30 patients,” said Bankova. “Unexpectedly, the interest was so high that we recruited and collected samples from more than 50 patients in just two months. In addition, we created a registry to collect longitudinal clinical information so we can understand the progression of this syndrome.”
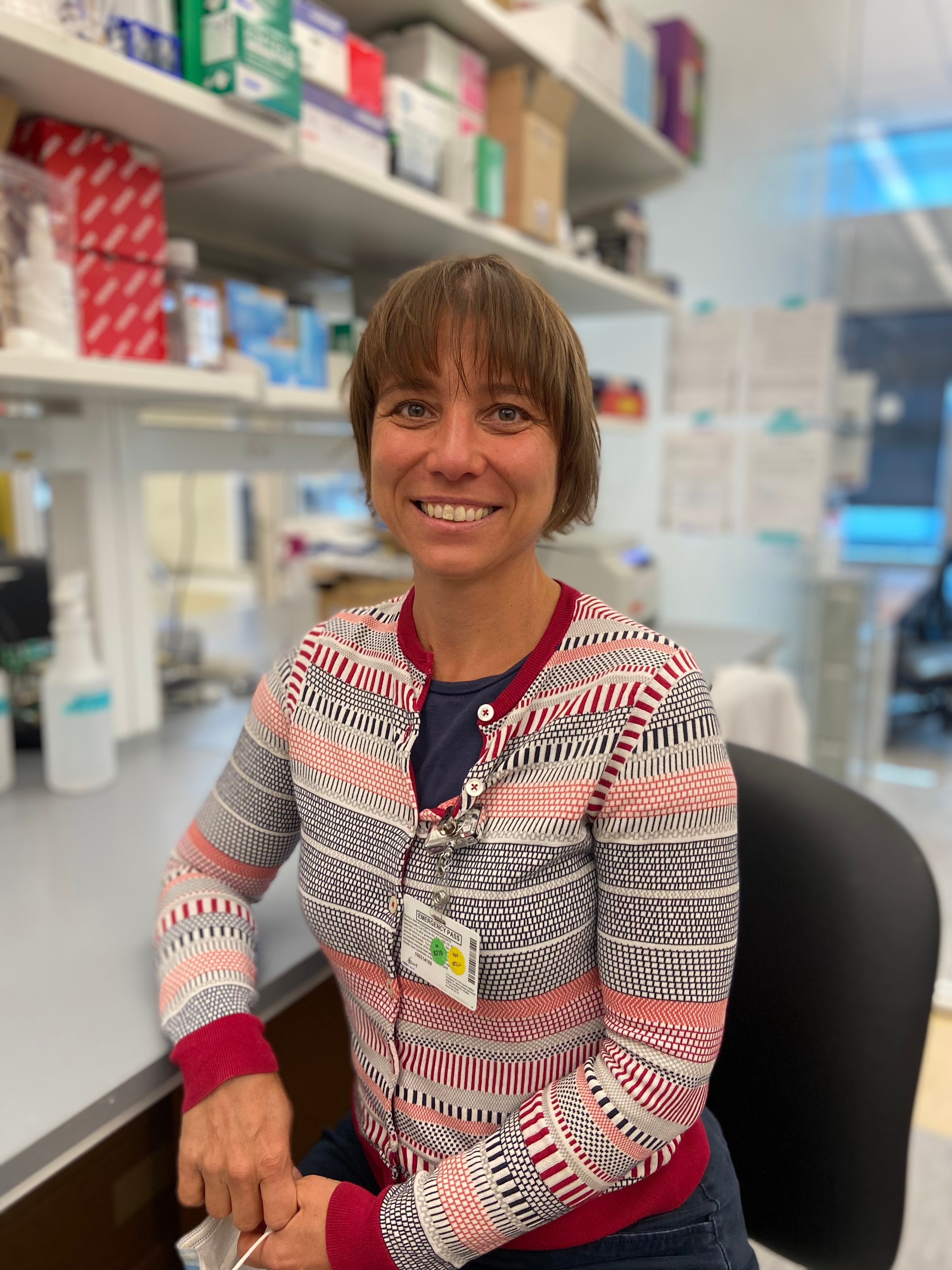
Combing through this registry of patients with post-COVID smell and taste disruption, Bankova and her team discovered that in 52% of these subjects, nasal dryness was associated with a loss of smell. The funding will allow the team to perform shotgun proteomics and high throughput lipidomics to deepen their understanding of the changes in the composition of the nasal lining fluid in people who have persistently disturbed smell and taste following COVID.
“The integrated analysis of protein, lipid mediator, and transcriptional analysis will allow the team to build a comprehensive hypothesis around why some people do not recover their sense of smell and taste following the virus,” she said.
A unique aspect of this pilot funding opportunity was the addition of a community engagement studio for each project. Each principal investigator presented their projects to a panel of local community leaders and patient advocates. The collaborative nature of the studios allowed the principal investigators to gain valuable feedback on the recruitment of patients and other best practices for disseminating the project’s outcome.
As these innovative projects demonstrate, support for early findings can help support advanced research into all aspects of the sensory systems. This important work is necessary for us to gain insight into the many ways we as humans connect to and enrich our environment using all our senses.
In addition to the above projects, seven other principal investigators were funded:
- James Naples, MD, Assistant Professor at Beth Israel Deaconess Medical Center (BIDMC)
- Divya Chari, MD, Lecturer at MEE
- Paulo Bispo, PhD, Assistant Professor at MEE
- Lana Vasung, MD, PhD, Assistant Professor at Boston Children’s Hospital (BCH)
- Lucy Shen, MD, Associate Professor at MEE
- Katherine Reinshagen, MD, Assistant Professor at MEE
- Samuel Mathias, PhD, Instructor at BCH
Read abstracts of the above projects.

