News & Highlights
Topics: Biomedical Science, Clinical & Translational Research, Diversity & Inclusion, Education & Training, Five Questions, Mentoring
Five Questions With Mike Super
Our Visiting Research Internship program mentor discusses his research at the Wyss Institute and the role of mentorship in supporting the next generation of translational researchers.
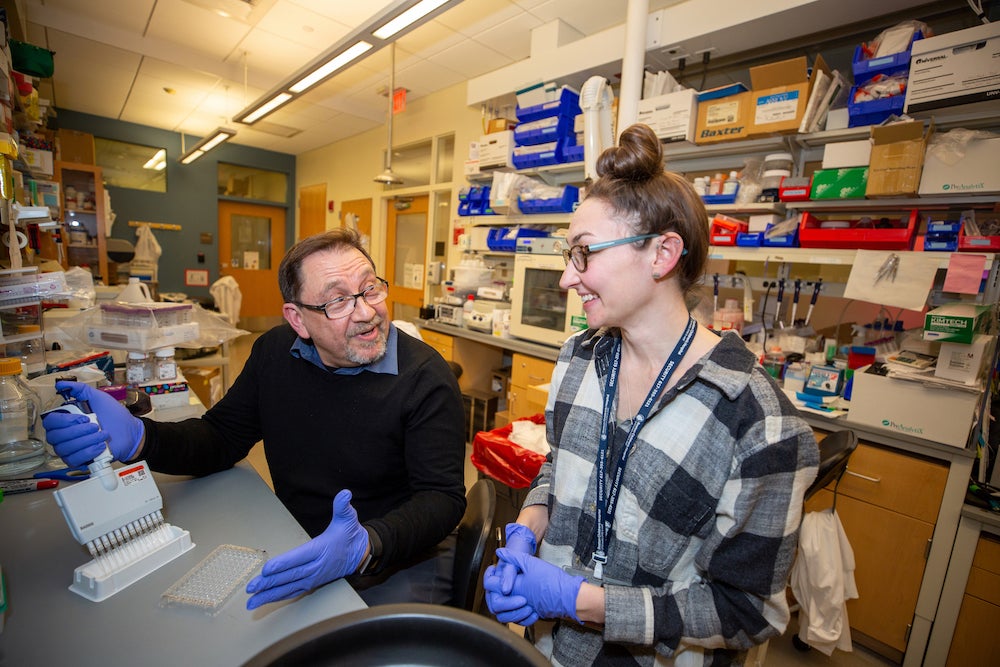
Michael Super, PhD, is lead senior scientist at the Wyss Institute for Biologically Inspired Engineering. Every summer he mentors medical students as part of Harvard Catalyst’s Visiting Research Internship program. Super’s research uses protein engineering to design therapeutics and diagnostic devices to treat cancer, infectious and immunological diseases. Prior to joining the Wyss in 2009, he spent 17 years in the biotechnology industry.
Who were some of your most meaningful mentors?
I grew up in South Africa and my father was a physician in a small town. He had to do himself what many different specialists in the Boston medical area do. I’ve also been mentored by some pretty strong women. My mother is a Holocaust survivor, which comes with strong survival skills. Along the way, I’ve had mentors like R. Alan Ezekowitz, with whom I did my postdoc at Children’s Hospital, Don Ingber, founding director of the Wyss, and Matt Turner, my doctoral thesis advisor at the University of London Institute of Child Health.
Why is the Visiting Research Internship Program so important to you?
Because these students didn’t luck out and grow up in say, Cambridge, Massachusetts. They’ve come here on a circuitous path, like I did. We get students who have tremendous drive, tremendous smarts, and skills, and not a lot of opportunity. Through VRIP, we give them a taste of what it’s like here. And they’ve all gone on to great things in academia and industry, which is very encouraging to see. One moment I’m writing a Rhodes Scholarship recommendation, the next, hearing about their latest success. Some I still collaborate with.
I think we give them a good grounding in medical science. For something to reach the clinic, they see all the animal work that has to be done, the lab work, and how it can all be pulled together. That’s part of mentoring.
“We get students who have tremendous drive, tremendous smarts, and skills, and not a lot of opportunity. Through VRIP, we give them a taste of what it’s like here.”
Your team’s dialysis-like device for diagnosing and treating sepsis is an incredible success story. From an animal study published in 2014, it took only five years to launch a company last fall that will bring it to market, and now you’re pursuing other applications for it. What lessons from this experience do you pass along?
One lesson is that you’ve got to keep going. I did my PhD thesis in the UK on the mannan-binding protein, which we found was missing in a group of children with frequent bacterial and fungal infections. Over the next 20 years, I did my postdoc at Children’s Hospital, and then went into industry, partly because I needed a green card, which was hard to get at Harvard at that time. When I joined the Wyss, Don Ingber was making a big push for us to find something that could bind to a broad spectrum of pathogens. It so happens that this protein I’d done my thesis on did exactly that. I designed and engineered the mannose-binding lectin (MBL), which is the basis of the dialysis-like therapy.
Soon after, DARPA (Defense Advanced Research Projects Agency) announced that they wanted to do a dialysis-like therapy for treating sepsis, which obviously fit us beautifully. We hit the four-year DARPA milestone in nine months. They’re difficult milestones, but we were very, very successful.
VRIP students have worked on many pieces of this project. They participate in all the DARPA team meetings. One moment they’re learning about proteins, then we are working on frog embryos and the design of a high- throughput screen to see the effect of compounds, drugs, and proteins on frog embryo development, and their impact on the microbiome.
We’ve been coming at this from many different directions. One student worked on a diagnostic based on MBL, published with us, and that diagnostic is part of the technology licensed to the company.
What vexing problems do you still want to solve?
We’re using the MBL technology to develop a vaccine against multiple different pathogens. We’re moving very quickly on it. So far we’ve found more than 120 different pathogens that can bind with the MBL.
My big worry is that vaccines, the solution to massive public health problems, are not just given short shrift, but campaigned against. I want to find a way — and maybe it’s through the pandemic we’re seeing in Asia now — for people to fear public health diseases again and stop this nonsense of not vaccinating.
What do you like to do in your off-work time?
When I’m not working, I try and focus on something completely different, whether it’s singing, digging in the garden, doing ceramics, or playing squash. I sing bass in the Longwood Chorus. I’ve been singing most of my life, but never at this level of talent! We have spring and winter concerts and sing in the hospitals. It’s healing for both singers and audience.

