News & Highlights
Topics: Clinical & Translational Research, Regulatory Guidance, Research Resources
When All Goes Quiet
Article showcased our work on the IRB Cede Review process (now SMART IRB). This piece led to national recognition of our work and shed new light on the nature of hearing injuries among Boston Marathon bombing victims.
Though she was standing 15 feet from the first blast, it wasn’t until the second blast occurred that Amanda North realized something was wrong. What she remembers next was an eerie silence, along with an ‘other-worldly’ calm that came over her.
Turning to help another injured spectator, Erika Brannock, who lay on the ground near the finish line, North didn’t realize until later, when she herself was treated, that the unusual quiet she was experiencing was a symptom of a perforated eardrum.
“My main goal was to help Erika, and hold her attention with my eyes so she would remain conscious. I didn’t know that my ear had been injured. It didn’t really occur to me that this was the reason why everything seemed quiet. I was just in a calm, almost relaxed, state trying to help,” North said.
North, one of 250 people injured in the April 15 Boston Marathon bombings, stayed with Brannock until help arrived.
Brannock lost her left leg, but North’s wounds were not life-threatening. After being released from Carney Hospital in Dorchester the day of the attack, and visiting Massachusetts Eye and Ear in Weymouth the next day, North, a high-tech executive, returned home to San Francisco.
A Silver Lining
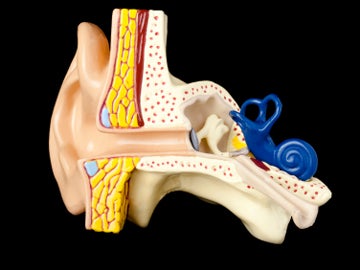
North’s ear injury, in which approximately 45 percent of her eardrum was perforated, healed after being treated with antibiotic drops and a patch on the eardrum, a common outcome for the injury. She was one of many victims that day who experienced trauma to their ears, which presented a unique opportunity for the Mass. Eye and Ear physicians who treated them that week. The sheer number of those injured prompted them to launch a three-year study of the effects of blast traumas, which they do not commonly see. While North is not a participant, dozens of other marathon bombing victims are taking part in the study, which investigators hope will illuminate this underresearched area.
Begun in late April by principal investigator Alicia Quesnel, HMS instructor in otology and laryngology at Mass. Eye and Ear, co-investigator Daniel Lee, HMS associate professor of otology and laryngology, and Aaron Remenschneider, a fifth-year resident in the HMS otolaryngology residency program, the study will examine post-blast trauma to the ear, and will follow approximately 100 patients who are receiving ongoing care and long-term monitoring at eight Boston-area hospitals.
Quesnel was one of many Mass. Eye and Ear otologists and audiologists who rushed to evaluate and treat patients who poured into Massachusetts General Hospital after the bombing. Also on call that day was Remenschneider, who treated dozens of patients.
“Because the attacks happened in the afternoon, we were fortunate in that we had a heads up that patients were probably going to be coming our way,” said Remenschneider. “So, there was a cadre of nursing staff, audiologists, other residents and attending physicians who stayed on to take care of the initial wave of patients.”
“As the on-call resident, I worked through the night, and began to see patients in intensive care at Mass General, many of whom had serious injuries, some of which required amputations,” Remenschneider said.
As the evening wore on, Remenschneider kept in touch with colleagues at Brigham & Women’s Hospital and Beth Israel Deaconess Medical Center, discovering that they, too, had been treating a range of ear injuries.
As the evening wore on, Remenschneider kept in touch with colleagues at Brigham & Women’s Hospital and Beth Israel Deaconess Medical Center, discovering that they, too, had been treating a range of ear injuries.
Traumatic Disorder
While otologists and audiologists at Mass. Eye and Ear often treat patients for trauma-related injuries, blast trauma patients are fairly rare. Patients being treated in connection with the bombings reported mild symptoms such as ear pain, disequilibrium, decreased hearing on one side, a “hollow,” or echo sound, in the ear, hyperacousis (increased sensitivity to sound) and tinnitus. Patients with sensorineural hearing loss were treated with oral steroids.
While some patients came in immediately, others called for appointments a few days later, realizing that something was not right with their hearing. For still others, the injuries were much more severe. Remenschneider treated patients who had extensive soft-tissue injuries to their ears and burns to the head and neck caused by shrapnel, beads and pellets.
“In one patient I treated, hot sparks from slags had entered and burned the ear canal, which completely destroyed his eardrum. This caused significant inflammatory response within the lining of the ear. He suffered maximum hearing loss because of this,” Remenschneider said.
In treating such an advanced injury, the immediate goal is to remove debris from the ear canal and clean the area.
“The other issue with tympanic membrane perforation is that skin can get blown into the ear canal and over time that can lead to a skin cyst, which can be destructive,” Remenschneider said.
In these cases, the primary goal is to try to remove skin debris and turn the edges of the eardrum out, so a cyst won’t form. Remenschneider added that, for these patients, reconstructive surgery is recommended several months later, once some measure of healing has taken place.
“Although we wanted to treat these patients early on, we let them know that we didn’t need to treat some injuries, such as a hole in the eardrum, right away. This made it easier for them to deal with their more serious injuries and also the emotional trauma that comes from such an experience,” Quesnel said.
While many of the area hospitals were seeing patients with a similar range of injuries—all of which were going to require ongoing care—the attending physicians at Mass. Eye and Ear faced the reality that they, and their colleagues at other hospitals, didn’t understand the nature of blast injuries.
Quesnel, Lee and Remenschneider consulted with faculty and read the current literature, deciding to contact military colleagues who have worked as ear, nose and throat specialists in combat settings.
In addition to their research expertise, the military physicians shared their experience of seeing veterans who came back from Iraq and Afghanistan.
Military Intelligence
“Although we commonly see these types of injuries—a patient suffering from sensorineural, or nerve-related, hearing loss or a perforated eardrum from a blow to the head, for example—we are not familiar with this mode of injury,” said Quesnel. “The outcomes will also be different in these circumstances. To be able to have this knowledge to help future patients is something that all the patients are very supportive of, and this is why they’ve agreed to participate in the study.”
Michael Hoffer, a neurootologist specializing in neurological disorders of the ear, is considered a leading expert in blast exposure injuries to the head. A director of the Spatial Orientation Center at the Naval Medical Center in San Diego and a Navy Representative to the Department of Defense’s Hearing Center of Excellence, Hoffer directs a lab that focuses on damage to the inner ear from noise, and from blunt and blast trauma.
Working with co-investigator Carey Balaban, vice provost for faculty affairs and professor of otolaryngology at the University of Pittsburgh School of Medicine, this research group has conducted studies of blast injury in combat. Recently, they published data that demonstrate the efficacy of treating hearing-related symptoms following a blast injury with N-acetylcysteine, an over-the-counter medicine. Their findings, said Hoffer, were directly applicable to the patients in Boston and the fertilizer plant explosion patients in West Texas, who were injured the same week.
On April 15, Hoffer saw a significant uptick in downloads of his study published in PLoS One in 2010, “Blast Exposure: Vestibular Consequences and Associated Characteristics.”
“Normally, the reported average yearly usage from PLoS One is 900 views per year; we had 540 in April alone, picking up dramatically six to eight hours after the bombing,” said Hoffer. “Clearly there is significant interest in understanding how to apply what we’ve learned in combat trauma to civilian populations. The Quesnel study is extremely important as it will give us our first domestic look into ear injuries seen after a blast and will help us assess diagnostic and treatment strategies.”
Quick Study
In addition to providing guidance on how best to help Mass. Eye and Ear patients, Hoffer helped Quesnel, Lee and Remenschneider review some of the protocol information for the study. It was later in the week following the attacks that the team at Mass. Eye and Ear decided to launch a study that would involve several Boston hospitals—five Harvard-affiliated hospitals, including Mass. Eye and Ear, and three additional sites.
The study will include several lines of inquiry: whether eardrum perforations will heal independently or ultimately require surgery, and also whether the characteristics of an eardrum perforation are different when caused by a blast or another cause; looking at the use of steroids as treatment for patients suffering from sensorineural hearing loss immediately after a blast; and examining the correlation between distance from the blast and the severity of hearing loss and eardrum perforation.
“Collecting good-quality data is going to be a time-consuming affair, so we are looking for ways to streamline this process. Here at Mass. Eye and Ear, we have nine otologists seeing patients and conducting follow-up, so tracking patients will be a bit of a challenge, but there’s some institutional support for us,” said Quesnel.
To aid data collection, Remenschneider is working to implement REDCap, a web-based application that supports data capture for research studies.
Upon submitting their research protocol to the Mass. Eye and Ear institutional review board 10 days after the attacks, Quesnel and Lee launched the process for IRB approval for the multisite study.
Traditionally, launching such a study would be a time-consuming, cumbersome process lasting weeks, even months. However, since 2009, Harvard Catalyst, the clinical and translational science center that supports research across Harvard University, has facilitated a framework for HMS-affiliated institutions to speed the review of human studies.
This new efficiency can be credited to the IRB cede review form, which allows an investigator to request a single IRB review.
Just one week after submitting the protocol to the Mass. Eye and Ear IRB, Remenschneider got to work using the Harvard Catalyst cede review form for the first time, requesting a single IRB review to seven area hospitals that included Brigham & Women’s, Beth Israel Deaconess, Mass General, Boston Children’s Hospital, Boston University Medical Center, Tufts Medical Center and Harvard Vanguard Medical Associates.
“Responses from the other IRBs came within a day or two, and they all accepted to cede review,” says Fariba Houman, director of the Human Research Protections Program at Mass. Eye and Ear.
“Procedures were refined through this discussion to maximize privacy of patient data. For example, age ranges would be collected instead of age of minors to safeguard the privacy of this small and very highly publicized group of victims,” Houman said.
Without the cede review process, the study would have been challenging to launch. Data captured while the patients remained in Boston following the blasts are critical to the success of this study.
Barbara Bierer, senior vice president of research at Brigham and Women’s and program director of regulatory knowledge and support at Harvard Catalyst, has spearheaded efforts to implement this resource for Harvard researchers.
“Our knowledge is always strengthened when Boston hospitals work together, and the IRB approval process can strongly impact the viability of a study. In this example, the investigators found this Harvard Catalyst resource and were able to expedite the multisite IRB process. This has been one of my team’s primary goals: to help minimize the regulatory burdens for researchers at Harvard—and beyond,” Bierer said.
Currently, the physicians at each of the participating hospitals are monitoring patients’ progress and will begin collecting outcomes during the next three months. As of early June, Quesnel reports that some patients’ eardrums have already healed, while others who have larger holes in their eardrums haven’t yet healed, an expected outcome because of the nature of their injuries.
“Depending on the size of the hole in the eardrum, patients are at risk for persistent perforation with associated hearing loss, unless they opt for surgery. And they are more susceptible to an infection if water gets in,” Quesnel said.
“This study would not have been possible without the cede review; there are just too many people to organize in a timely fashion, so it was really the key for this study,” Quesnel said. “This has truly been a collaborative effort among the community of Boston otologists and otolaryngologists. Because of their willingness to come together, we are able to work towards the same goals, which will allow us to further our knowledge of this important research area and help patients receive the best care possible.”
“It’s a privilege—and humbling at the same time—to be able to take care of patients who have been through something like this and conduct this research. It’s so different from what the majority of our patients are coming in for. They’re certainly a very special patient population for us,” she said.

